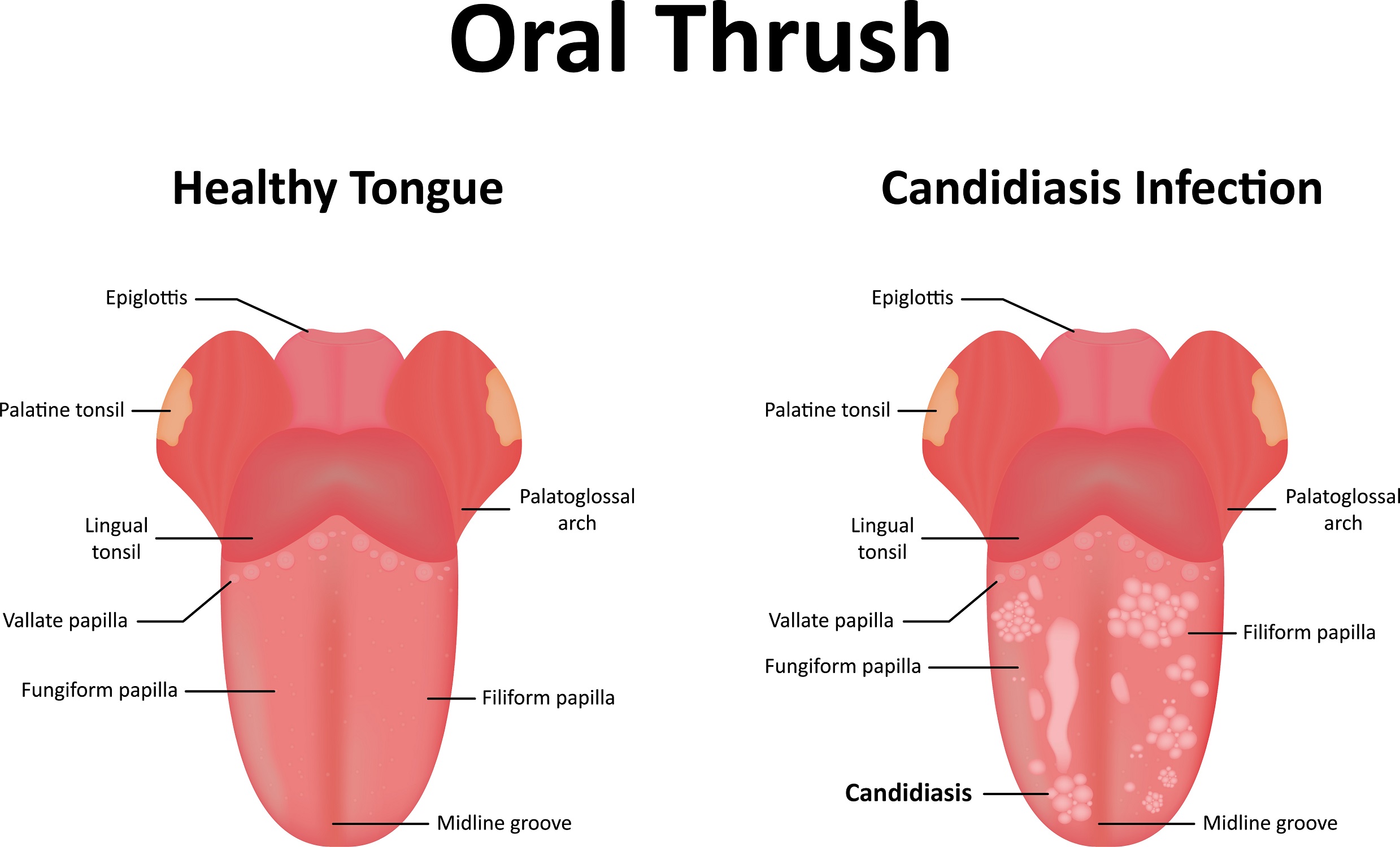
Oral candidiasis, also known as oral thrush, is a common fungal infection that occurs in the mouth. It is caused by the overgrowth of a naturally occurring yeast found in the mouth, digestive tract, and skin called Candida albicans. Candida is usually harmless, but certain conditions can cause it to multiply uncontrollably, which leads to oral thrush.
Symptoms of Oral Thrush
There are several distinctive symptoms of oral thrush that can vary in severity. The most recognizable sign is the appearance of white, creamy patches on the tongue, inner cheeks, roof of the mouth, gums, and tonsils. These lesions tend to look like cottage cheese and can sometimes be wiped off, revealing red, raw, and possibly bleeding areas underneath.
Additional symptoms of oral thrush can include:
- Redness and soreness inside and at the corners of the mouth.
- A cottony feeling in the mouth.
- Loss of taste.
- Pain or difficulty swallowing, especially if the infection spreads to the esophagus
Causes and Risk Factors
Our immune systems keep the balance between beneficial bacteria and things like Candida in our bodies. When the balance is disrupted, Candida can multiply, leading to oral thrush. This imbalance can be caused by several factors:
Weakened Immune System: People with immune systems, such as those with HIV/AIDS, undergoing cancer treatments, or taking immunosuppressive medications, have higher risks of developing oral thrush.
Medications: The use of antibiotics can kill beneficial bacteria that keep Candida growth in check. Similarly, corticosteroids, especially those used in inhalers for asthma or chronic obstructive pulmonary disease (COPD), can increase the risk as well.
Poor Oral Hygiene: Neglecting oral hygiene creates an environment where fungal growth like Candida will thrive.
Medical Conditions: Conditions like diabetes, dry mouth, and hormonal changes during pregnancy can also increase susceptibility to Candida overgrowth.
Lifestyle Factors: Smoking, wearing ill-fitting dentures, and a diet high in sugar can further increase the risk of oral thrush.
Diagnosis
Typically, your dentist or other healthcare provider will perform a simple visual examination when diagnosing oral thrush. The characteristic white lesions described above are usually enough for a diagnosis. In some cases, they may need to take sample from the lesions and examine it under a microscope to confirm that it’s Candida.
For more severe infections that may have spread to the esophagus, additional tests like a throat culture or endoscopy might be necessary.
Treatment for Oral Thrush
Treatment for oral thrush usually involves the use of antifungal medications, which can vary depending on how severe the infection is and the patient’s overall health. Common antifungal treatments include:
- Nystatin: Available as a mouthwash, lozenge, or topical cream.
- Clotrimazole: Typically taken as a lozenge that dissolves in the mouth.
- Miconazole: Available in a dissolvable tablet or topical form.
- Itraconazole and Fluconazole: These medications can be taken orally or administered intravenously in more severe cases
The duration of treatment usually spans one to two weeks, and it is crucial to complete the entire course of medication to keep oral thrush from coming back.
Preventing Oral Thrush
Preventing oral thrush involves adopting good oral hygiene practices and managing any underlying health conditions. Here are some tips to reduce the risk:
- Practice Good Oral Hygiene: Brush your teeth at least twice a day and floss daily. Regular dental check-ups are important, especially if you have diabetes or wear dentures.
- Rinse Your Mouth: If you use corticosteroid inhalers, always rinse your mouth or brush your teeth afterward.
- Limit Sugar Intake: Reduce the amount of sugar and yeast-containing foods you’re consuming, such as bread, beer, and wine, which can promote Candida growth.
- Quit Smoking: Smoking changes the balance of microorganisms in your mouth, making you more susceptible to infections.
Complications of Untreated Oral Thrush
While oral thrush is usually very treatable, leaving it untreated often leads to complications, especially in people with weakened immune systems. The infection can spread to the esophagus, causing esophagitis, which may lead to pain and difficulty swallowing. In severe cases, Candida can enter the bloodstream and spread to other parts of the body, such as the eyes, brain, or heart, which can lead to life-threatening conditions.
When to See a Doctor
If you experience persistent symptoms of oral thrush or have a weakened immune system, seek medical attention as soon as you can. Catching and treating things like this early can prevent complications and promote a quicker recovery.
Defending Against Oral Thrush
Oral thrush is a common but very manageable condition. Recognizing the symptoms, understanding the causes, and adhering to preventive measures can significantly reduce the risk of developing this fungal infection. If you suspect you have oral thrush, talk to your healthcare provider for appropriate diagnosis and treatment.